Congestive prostatitisis a pathological process in the prostate caused by obstruction. Pathogenic flora was not detected; Microscopy of prostatic secretions, semen, and urine may reveal leukocytes. Symptoms include constant pain in the perineum and difficulty urinating. Diagnosis is based on the results of biomaterial bacterial culture and TRUS. There is no single treatment regimen for congestive prostatitis; massage, physical therapy, antibiotics and alpha blockers are prescribed. An individual approach is needed, taking into account the existing symptoms. If conservative treatment fails, surgery is possible.
General information
Prostatitis can be infectious due to the presence of pathogenic or stagnant microflora, associated with blood congestion, semen stagnation, and prostatic secretions. Congestive or congested prostatitis (vegetative genitourinary syndrome, prostatic hypertrophy) is an outdated name. Modern specialists in the field of urology often use the term "chronic non-inflammatory pelvic pain syndrome" (CPPS). Prostatitis occurs in 25% of men aged 35-60 years, inflammation due to congestive processes accounts for 88-90% of all cases. The congestive form of the disease is supported by pathogens in the L form, immobilized on biofilms and not detected by conventional methods.
reason
The cause of congestive prostatitis may be related to both glandular and extraprostatic factors. The exact cause is unknown, it may be due to stagnation of secretions in the prostate or as a result of venous congestion in the pelvic organs and scrotum. Some urologists consider this condition to be psychogenic. The boundary between bacterial and bacterial inflammation is very arbitrary; with immunosuppression of any origin, due to the addition of secondary microflora, the process becomes infectious. Congestive prostatitis is caused by:
- Internal urinary causes. Functional or structural pathology of the bladder: cervical obstruction, inability of the external sphincter to relax during bowel movements, impaired bladder muscle contractility contributing to urinary retention and compression of blood vessels, blood stagnation. Prostatic hyperplasia and tumors, urethral strictures, and obstructive bladder stones are also considered potential causes of venous obstruction.
- Compression. Blood circulation is obstructed due to the retroperitoneal tumor compressing the venous plexus, metastasizing and the intestinal loops filling with stool (constipation). The vessels of the genital plexus dilate, blood flow slows down, tissues are deprived of oxygen and are replaced by structures that no longer function. Part of the blood is deposited and stops circulating.
- Behavioral factors. Refusing sexual activity, irregular ejaculation, and using interrupted sexual intercourse as a means of preventing unwanted pregnancy cause blood flow and swelling of prostate tissue. During ejaculation, this gland is not completely drained. Continuous masturbation can lead to congestive prostatitis, because. . . To develop an erection, blood flow to the genitals is necessary.
Risk factors include low physical activity, hypothermia and overheating, and a poor diet with mainly spicy, smoked foods. Alcohol and nicotine affect the tone of the vascular wall, disrupting redox processes and permeability, causing swelling. The main prerequisite for the formation of congestive prostatitis affecting all organs of the male genital area (water sac, testicles) is considered to be anomalies of the pelvic vascular system - valvular insufficiency, Congenital weakness of the venous wall.
Pathogenesis
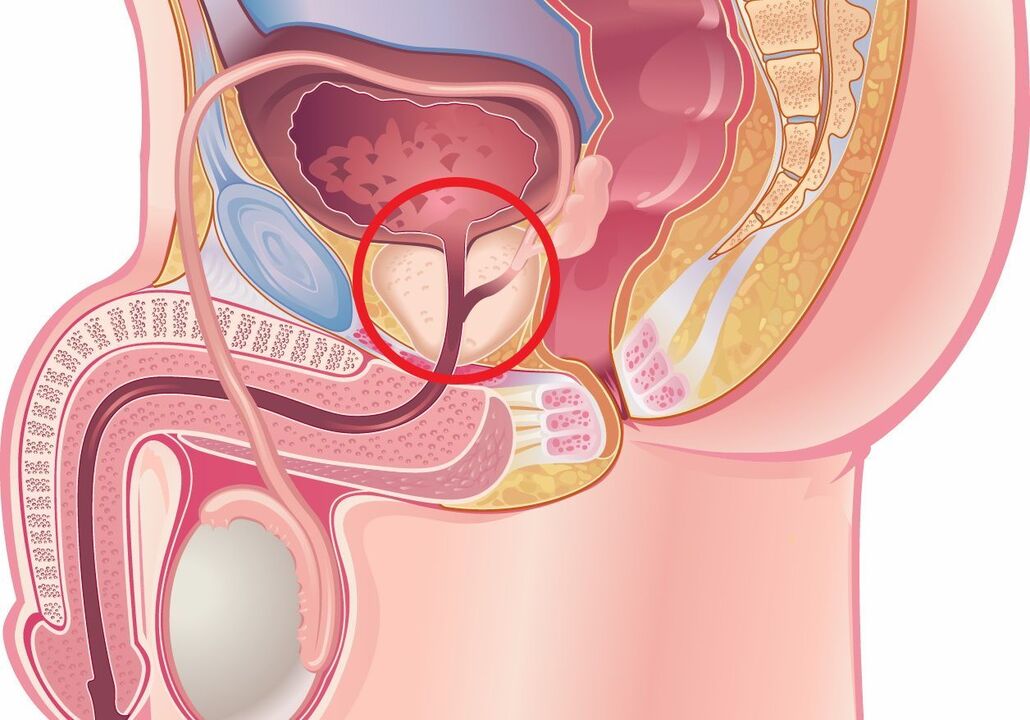
The periphery of the prostate consists of ducts with a poorly developed drainage system, which impedes the escape of secretions. As the prostate enlarges with age, the patient will experience reflux of urine into the prostatic duct. It is noted that many men with prostatitis are more susceptible to allergies. Scientists believe that such patients may also have autoimmune-mediated inflammation due to previous infections.
Urinary reflux is promoted by urethral stricture, bladder dysfunction, and BPH. Backflow of sterile urine can even lead to chemical irritation and inflammation. The process of tubular fibrosis is initiated, creating favorable conditions for prostatic stone disease, increasing intratubular obstruction and stagnation of secretions. Inadequate drainage of the acini will cause an inflammatory response, increasing swelling accompanied by the appearance of symptoms. The condition is aggravated by congestion (stasis) of blood in the pelvis.
Classify
The general classification of prostatitis includes acute (I) and chronic (II) bacterial forms. Type III includes subgroups IIIa – inflammatory CPPS and IIIb – non-inflammatory CPPS. Congestive prostatitis is considered a manifestation of CPPS when there is no inflammatory response (IIIb). There is a clinical distinction that takes into account the morphological and pathophysiological features of the disease:
- First stage.Characterized by the predominance of secretory, migratory processes, arterial and venous hypertension, leading to microvascular damage and destruction of glandular tissue. These changes are noted in the first years after the onset of the disease. The clinical picture in the early stages is the most obvious.
- Second stage.The initial processes of connective tissue proliferation develop and symptoms gradually subside. Due to the formation of thrombus, microcirculation is affected, aggravating sclerosis. At this stage, most patients experience sexual dysfunction: the ability to have an erection and the intensity of orgasm weakens, premature ejaculation develops or, conversely, the man has difficulty achieving sexual intercourse. reach orgasm.
- Third stage. Severe sclerotic changes are typical. It has been shown that connective tissue proliferation is stimulated not only by inflammation but also by ischemia accompanying congestive prostatitis. Complaints of dysuria are typical and renal involvement in the pathological process is noted.
Symptoms of congestive prostatitis
The disease manifests with many different symptoms. Most patients describe the pain as a constant feeling of discomfort in the perianal area, scrotum, or penis. Some note that the pain in the perineum is worse when sitting. The level of pain can vary - to the lower back, inner thighs, coccyx. Swollen glands often cause difficulty starting urination and weaken the urine flow. A type of vasculitis that is often accompanied by hemorrhage - the appearance of blood in the semen.
Symptoms of bladder irritation include urinary urgency and frequency. With long-term pathology, depressive disorders develop. It is still debated whether psycho-emotional characteristics lead to perineal discomfort or, conversely, whether pain from prostate swelling affects the mental state of men. Increased temperature accompanied by chills indicates the transition of bacterial congestive prostatitis to infection and the need to begin treatment of the pathology.
symptoms
Congestive prostatitis when supplemented with microflora can become acute bacterial. Nearby organs and structures can participate in the inflammatory process: vesicles, bladder, testicles. The role of the prostate is to produce fluid for sperm, usually it has a special composition that functions to protect male germ cells. Inadequate nutrient intake and changes in the biochemical properties of prostatic secretions certainly affect the quality of ejaculation; Men with congestive prostatitis are often diagnosed with infertility.
When the organ is severely swollen, part of the urine after urination remains in the bladder, leading to the formation of a pathological reflux of urine into the ureters and kidney collection system. In response to reflux, hydronephrosis and persistent pyelonephritis may occur with impaired renal function. 50% of men suffer from sexual dysfunction: pain during ejaculation, painful intercourse, uncomfortable erection at night, causing quality of life to decline and negatively affecting the marital relationship.
Diagnose
Determining the origin of symptoms is important for effective treatment of congestive prostatitis, therefore various questionnaires have been developed to aid in diagnosis: I-PSS, UPOINT. These questionnaires are available in Russianized form, they are used by urologists and endocrinologists in their practice. To rule out myofascial syndrome, consultation with a neurologist is required. On palpation, the prostate gland is enlarged, moderately painful, the congested nature of the disease is manifested by rectal varicose veins. Diagnosis of congestive prostatitis includes:
- Laboratory testing. A microscopic examination and culture of the prostate fluid were performed. A mildly increased white blood cell count under the microscope and a negative bacterial culture confirmed bacterial congestive inflammation. PCR testing is performed to rule out the sexually transmitted nature of the disease. In the third portion of urine after massage, a more pronounced increase in leukocytes was detected. To rule out bladder tumors, a urine cytology test may be performed; in patients over 40-45 years of age, a PSA blood test is reasonable.
- Visual research methods. The main instrumental diagnostic method is still TRUS, bladder ultrasound. The results of cystourethrography are informative in confirming bladder neck dysfunction, detecting intraprostatic urinary reflux and ejaculation, as well as urethral stricture. In case the jet is noticeably weaker, urine flow measurement is performed. Pelvic floor muscle tension was assessed by videodynamic study.
Differential diagnosis is made with bladder carcinoma, BPH, interstitial cystitis. Similar manifestations are observed in urinary tuberculosis and urethral stricture, as these pathologies are also characterized by lower abdominal pain, dysuria and dysuria symptoms. Congestive prostatitis is distinguished from bacterial prostatitis, in addition, all pathological processes accompanying CPPS in men must be excluded.
Treatment of congestive prostatitis
Patients are encouraged to normalize their sexual life, as regular ejaculation helps drain the acini and improve microcirculation. Interrupted or prolonged sexual intercourse, causing obstruction, is unacceptable. Certain products have been identified as increasing the chemical positivity of urine - their consumption leads to increased symptoms of congestive prostatitis. Spices, coffee, sauces, smoked foods, alcoholic and carbonated drinks should be limited, or better yet, excluded. Treatment of congestive prostatitis can be conservative and surgical.
Conservation therapy
The treatment regimen is selected individually, depending on the common symptoms. In many patients, improvement occurs after taking antibacterial drugs, which is explained by incomplete diagnosis of underlying infections. For cases where the urine flow is slow and requires exertion, alpha blockers are prescribed. Urinary urgency is neutralized with anticholinergic drugs. 5-alpha reductase inhibitors have been shown to reduce the severity of clinical manifestations by reducing macrophage and leukocyte responses and their migration into areas of inflammation.
Pain relievers, nonsteroidal anti-inflammatory drugs, and muscle relaxants can help relieve pain and muscle spasms. It is reasonable to include in the treatment regimen drugs that normalize microcirculation – phlebotonics (venotonics). If the stagnation leads to androgen deficiency, they will use hormone replacement therapy. Patients with anxiety-hypnotic disorders and depression should consult a psychiatrist to choose the optimal antidepressant.
When suffering from congestive prostatitis, physical therapy courses help normalize men's health. They use laser and magnetic therapy, electrophoresis, etc. v. Spa treatments help reduce symptoms of dysuria and improve sexual function: drink alkaline mineral water, apply paraffin and mud, and take massage baths. In some patients, normalization of health is noted when performing exercise therapy to reduce tension in the pelvic muscles. Prostate massage does not replace natural ejaculation but improves blood circulation and drainage of the organ.
Minimally invasive treatment method
If conservative treatment is unsuccessful, high-tech interventions are considered - transurethral prostatectomy, high-intensity focused ultrasound ablation. The most effective is rectal hyperthermia - a non-invasive method based on the principle of thermal diffusion (prostate is exposed to unfocused microwave energy). Heat increases tissue metabolism, reduces symptoms of congestion and has a neuropathic pain-relieving effect. Data on the effectiveness of these procedures in the treatment of congestive prostatitis are limited.
Prognosis and prevention
The prognosis for life is favorable, but chronic pelvic pain is difficult to treat. Sometimes congestive prostatitis will go away on its own over time. Prolonged circulatory disorders lead to sclerosis of the glandular tissue, manifested by a decrease in sperm parameters. The prognosis of congestive prostatitis largely depends on the patient's compliance with all recommendations and lifestyle changes.
Prevention includes playing sports, avoiding heavy lifting, normalizing sexual intercourse and avoiding coffee and alcohol. When working sedentary, take breaks to exercise and use pillows. Prioritize loose underwear and pants. Patients were periodically observed and evaluated by a urologist for prostatic secretions for inflammation and ultrasound, and, if necessary, received antibacterial treatment and prostate massage.




































